The Relation between Ambient Temperature and Asthma Exacerbation in Children: A Systematic Review
Hamid Reza Shoraka1,3, Moslem Taheri Soodejani1, Omid Abobakri1, Narges Khanjani2*
1Dept. of Epidemiology and Biostatistics, Kerman University of Medical Sciences, Kerman, Iran
2Environmental Health Engineering Research Center, Kerman University of Medical Sciences, Kerman, Iran
3Vector-borne Diseases Research Center, North Khorasan University of Medical Sciences, Bojnurd, Iran
Abstract
Background: Asthma is one of the most common chronic non-communicable diseases which is seen more in the developed than developing countries of the world. Recurrence and exacerbations of the disease are common among patients and often lead to hospitalization and therapeutic interventions. Ambient air temperature might be related to the relapse of asthma. This review was conducted to investigate the relation between ambient temperature and exacerbations of asthma in children.
Methods: Related articles were searched in PubMed, Web of Science, Science Direct, and Scopus databases with appropriate keywords and no specific limitation on October 1, 2018. Initially, the relevance of the articles was examined using the title and abstract. Out of 2633 articles, 23 articles were eligible according to the inclusion and exclusion criteria.
Results: Fourteen studies had reported inverse relations; and showed as the temperature dropped, the number of asthma attacks increased in children. Nine papers observed a relation between hot weather and asthma attacks, 3 studies reported a relation between temperature differences and asthma attacks, and two studies did not show any relation. Some studies suggested the increased incidence of asthma in the 5-14 year old age group was associated with the start of the school year and probably due to the spread of viral diseases, not temperature changes.
Conclusion: Extreme temperatures are likely to cause exacerbation of childhood asthma.
Introduction
Asthma is one of the most common chronic airway and non-communicable diseases worldwide and its prevalence has increased in recent years1. This disease is characterized by chronic inflammation and obstruction of the airways. According to the WHO report, 235 million people suffer from this disease2.
Recurrence and exacerbations of this disease are common among patients, which often leads to hospitalization and therapeutic interventions for improving lung function3. Several studies have been conducted to investigate the relation between air pollutants such as ozone and fine particulate matter and the progression and exacerbations of asthma. There is also evidence that exposure to environmental factors such as ambient temperature is associated with recurrence of asthma4, and even deterioration and death due to respiratory failure5, 6.
Average global temperature has increased 0.85 ?C , between 1880 and 20127. Nowadays all world countries are affected by global warming and its effect is not limited to a specific region of the world8.
Air temperature may directly or indirectly be related to the recurrence of asthma. Cold air may directly affect airways and cause hyper-responsiveness. It might also indirectly trigger asthma by predisposing people to viral diseases, or air pollution. Air conditioners used in warm weather may also trigger the recurrence of asthma9. Several studies have been conducted in different countries to investigate the relation between ambient temperature variations and the incidence and/or recurrence of asthma. Studies have reported clusters of asthma recurrence and hospitalization in some seasons10. Children are one of the sensitive groups affected by environmental factors. These factors might cause asthma recurrence and hospitalization in sensitive children11.
Understanding the environmental factors that trigger asthma recurrence and hospitalization in children can help prevent these attacks by modifying lifestyle or reducing exposure to these environmental factors12. Various studies have reported different results about the role of ambient temperature on the occurrence of asthma. These studies have been conducted in different geographic, social and racial regions and have examined the effect of low or high temperatures, or heat/cold waves, on the exacerbation of asthma13, 14. These studies have reported various associations and it is necessary to provide an overall conclusion from these studies to help public health policymaking. Although a systematic review was recently conducted about ambient temperature and childhood asthma by Xu et al15, but this review did not include some articles4, 16-29.
This review study was conducted to investigate the relation between ambient temperature and asthma focusing on recurrence and exacerbation of the disease in children.
Materials & Methods
Inclusion Criteria
Studies were included in this review if they had considered at least one temperature index as an exposure, had evaluated the age group under 17 years separately, the outcome was investigated in humans, and recurrence or hospitalization due to exacerbation of asthma was reported as a consequence. Also, papers were included which had included at least one year data.
Inclusion Criteria
PubMed, Web of Science, Science Direct, and Scopus databases were searched for relevant articles. No time limit was implemented.
The keywords "temperature", "weather", "climate"," heat", "hot", "cold" and "ambient temperature" were used as exposure terms and "hospital*","admission*", "emergence*", "exacerbation" and "asthma" were used as outcome terms. The final search was done on October 1, 2018. In order to retrieve all related articles which included various age groups, we did not use “Children” as a keyword. Hence, we screened full-text articles to see if they had included children as a separate category.
Study selection
After searching different databases, the titles and abstracts of the retrieved articles were imported into EndNote software and duplicates were removed based on title, author and year of publication.
Initially, the relevance of the articles was examined based on title and abstract. Out of 2633 articles, 88 were selected for full-text evaluation. The full-text articles were evaluated using the inclusion and exclusion criteria.
Result
After screening through several steps, shown in Figure 1, 23 articles were selected for the review. The characteristics of these articles are summarized in Table 1. The studies were from different parts of the world including Europe, America and Asia, but no study was conducted in Africa. The studies had been conducted in 12 countries.
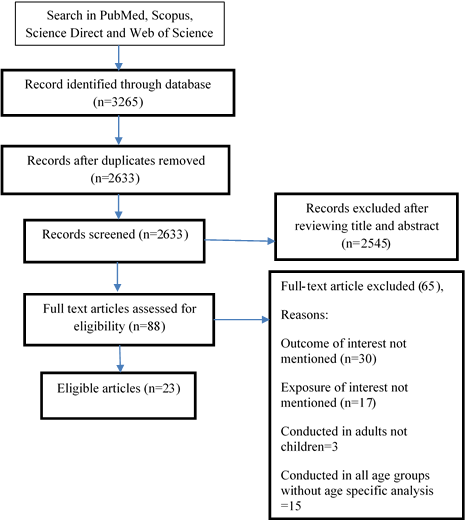
Figure 1: Search results and study selection
Table 1. Summary of the studies included in this systematic review
| ID | First Author, Year, location | Population size | Study period | Ages | Outcome definition | Exposure definition | Study type | Köppen−Geiger Climate Classification | Dominant gender | Lag time | Other variables included | Statistical analysis | Main results |
| 1 | De Souza, 2015, Brazil(17) | 5844 | 2008-2010 | <9 | ICD10-(J45) | Daily Mean Temperature (DMT) | Ecologic | A | NR? | 0-30 | Humidity, Rain fall, Wind Speed, O3 | Pearson Correlatio | Daily hospital admissions showed significant negative correlations with DMT (r=−0.214, P<0.001), |
| 2 | Fitzgerald, 2014, USA(4) | 396043 | 1991-2007 | <17 | ICD9-(493.00) | Daily Mean Temperature | Ecologic | C | Female | 0-4 | PM2.5-Sex -Race | GAM | Decrease in admissions during a cold spell in the winter months for all subgroups. A mean decline of 4.9 % in asthma admissions happened statewide (95 % CI -7.8, -1.9 %). |
| 3 | Hashimoto, 2004, Japan(12) | 5559 | 1998-2002 | 2-15 | Physical findings such as dyspnea with wheezes | Daily Min, Max and Mean Temperature | Ecologic | C | NR | 3 | Barometric Pressure, Humidity/Vapor Pressure, Wind Speed | Logistic Regression | The rapid decrease of temperature within a 3-day period can increase the risk of asthma attacks. β=0.05, CI= 0.02–0.07 |
| 4 | Lam,2016, Hong Kong(31) | 2402 | 2004-2011 | <15 | ICD9-(493.00) | Daily Mean Temperature | Time -Series | C | NR | 20-30 | Air Pollutants, Solar Radiation, Wind Speed | GAM, DLNM | Asthma admissions increased at high temperatures in the hot season and at low temperatures in the cold season RR=1.19 |
| 5 | Liu,2007, China(23) | 445 | 2000-2004 | 0-14 | Diagnosis by clinicians | Monthly Mean Temperature | Historical Cohort | C | Male | NR | Air Pressure, Relative Humidity, Wind Speed | Linear Regression Analysis | Higher incidence was related with lower temperature, (r =-0.320 , P < 0.05) |
| 6 | Nastos,2006, Greece(24) | 2764 | 2001-2003 | 0-14 | Admitted with the diagnosis of “asthma”, “asthmatic bronchitis” or “wheezy bronchitis” | Daily Min, Max and Mean Temperature, Diurnal Temperature | Time-Series | C | Male | NR | Water Vapor Pressure and Cold Anti Cyclonic | Pearson Correlation | Low temperature, significantly correlated with an increase in the number of asthma admissions |
| 7 | Soneja,2016, USA(34) | 119523 | 2000-2012 | <17 | ICD9-(493.00) | Daily Max Temperature, Extreme Heat | Case-Crossover | C | Female | 0-2 | Sex, Race | Conditional Logistic Regression | Exposure to extreme heat events was associated with a 3 % increase in the risk of hospital admission for asthma (Odds Ratio: 1.03) |
| 8 | Wasilevich,2012, USA(27) | 4804 | 2000-2001 | 3-18 | ICD9-(493.00–493.99 | Hourly Min, Max and Mean Temperature | Case-Crossover | D | Male | NR | Relative Humidity, Barometric Pressure, Wind Speed, Thunderstorm Activity and Air Pollutant | Conditional Logistic Regression | The case crossover study showed a statistically significant inverse relation between ED visits and maximum 24-hour temperature change after adjustment for climatic factors, RR=0.972, P = 0.01 |
| 9 | Xu,2013, Australia(35) | 13324 | 2003-2009 | 0-14 | ICD10-(J45) | Daily Min , Max and Mean Temperature | Ecologic | C | Male | 0-1, 0-13, 0-21 | PM10, 03 | Poisson Linear Regression | Male children and children aged 0–4 years were particularly sensitive to hot temperature (RR= 1.61 CI=1.22 to 2.14), and children aged 10–14 years were particularly sensitive to cold temperatures (RR=1.96 ,CI=1.03 to 3.50) |
| 10 | Altzibar,2015, Spain(16) | 59500 | 2004-2009 | <15 | ICD9-(493.00) | Daily Min , Max and Mean Temperature | Ecologic | C | Male | NR | Age, Sex, Air Pollutant, Relative Humidity and Flu Status | Pearson Correlation | Asthma exacerbations were correlated negatively with temperature. (r=-0.485 CI=-0.543;-0.423) |
| 11 | Ehara,2000, Japan(18) | 205 | 1997 | 1-16 | Asthmatic symptoms, such as wheezing and expiratory stridor | Daily Diurnal Temperature | Ecologic | D | Male | 1 | Barometric Pressure and relative Humidity | Mann–Whitney U-test | Diurnal difference between maximum and minimum temperatures of 1 day before admissions was larger than that of 1 day before days with no admissions P=0.02 |
| 12 | Grech,2002, Malta(20) | 2916 | 1994-1998 | 0-59 | Diagnosis of asthma or wheezy bronchitis | Monthly Min , Max and Mean Temperature | Ecologic | C | NR | NR | Age Group | Spearman Correlation | Ranked mean monthly ambient temperatures correlated significantly with monthly admissions in the pediatric cohort (r= -0.71, p<0.0001) |
| 13 | Hervas,2015, Spain(30) | 371 | 2007-2011 | 5-14 | ICD9-(493.0-493.9) | Monthly Min, Max and Mean Temperature | Longitudinal Retrospective | C | Male | 30-60 | Water Vapor Pressure, Relative Humidity | Multivariate linear Regression | The Regression equation showed a 7.3% increase in the number of monthly asthma exacerbations for each degree decrease in temperature. (β=27.2, P<0.0001) |
| 14 | Ivey,2003, Trinidad and Tobago(22) | 45842 | 1997-1999 | 0-65 | Diagnosis of acute asthma and received bronchodilator nebulization | Daily Min and Diurnal Temperature | Ecologic | A | NR | 1 | Relative Humidity, , Barometric Pressure, Wind Speeds | Multiple Regression | Results of multiple regression indicated that temperature difference (P<0.001) : and minimum temperature (P<0.001) were predictors of pediatric visits |
| 15 | Nastos,2008, Greece(33) | NA | 1978-2000 | 0-14 | Diagnosis of “asthma,” “asthmatic bronchitis” or ”wheezy bronchitis,” | Monthly Diurnal Temperature | Ecologic | C | NR | 0-3 | Relative Humidity, Absolute Humidity and Wind Speed | Generalized Linear Models | There was a negative relation mean monthly air temperature and asthma admissions in the age group 0 -4 years (B= −0.0376, P= <0.0001) |
| 16 | Garty,1998, Israel(19) | 1076 | 1993 | 1-18 | Diagnosed as having an acute asthma attack | Daily Min and Max Temperature | Ecologic | C | Male | NR | Barometric Pressure, Relative Humidity, Air pollutant | Pearson Correlation | ER visits showed a negative correlation with minimal temperatures (r = -0.45) and maximal temperatures (r = -0.41) |
| 17 | Ivey,2001, Trinidad and Tobago(21) | 27848 | 1997 | <16 | Diagnosis of acute asthma and received bronchodilator nebulization | Daily Mean Temperature | Retrospective Ecologic Study | A | Equal | NR | Rainfall, Relative Humidity, Sex | Multiple Regression | Increased asthma visits in children were associated with increased temperature β= 0.14270, P= 0.009 |
| 18 | Li,2016, China(32) | 17022 | 2007-2013 | 0-14 | Diagnosis by clinicians | Daily Min, Max and Mean Temperature and TVN* | Ecologic | C | Male | 10 | Sex, Relative Humidity | Poisson Generalized Linear Regression | A 1o C increase in temperature variation was associated with a 4.2% (95% CI 0.9-7.6%) increase in the number of hospital visits for childhood asthma |
| 19 | Mireku,2009, USA(36) | 25401 | 2004-2005 | 0-18 | Diagnosis by clinicians | Daily Min, Max and Mean Temperature | Retrospective Ecologic Study | D | NR | 0-5 | Humidity, Barometric Pressure, Air pollutant | Time series | Interday changes in temperature from 1 day before asthma attack increased ED visits, with a 10°F increase being associated with 1.8 additional visits (P = 0.006). |
| 20 | O’Lenick,2017, USA(25) | NR | 1993-2012 | 0-19 | ICD9-(493.0-493.9) | Daily Min, Max and Mean Temperature | Ecologic | C | Male | 0-7 | Sex, Race, Insurance Status | Poisson generalized linear models | Estimated RRs for T max and pediatric asthma ED visits were positive and significant for lag days 1–5, with the strongest single-day association observed on lag day 2 (RR=1.06, 95% CI: 1.03, 1.09) |
| 21 | Zaninovic,2001, Croatia(29) | 84 | 1984 | Not Reported | Not Reported | Daily Min, Max and Mean Temperature | Ecologic | C | NR | 0-7 | Humidity, Barometric Pressure and Wind Speed | Spearman Correlation | Negative correlation coefficients between asthmatic attacks and mean, maximum and minimum air temperatures appeared on most days. The results considered together point at cold, clear and dry winter anticyclonic situations as dangerous for the asthmatics |
| 22 | Palusci, 1998,USA(26) | 6741 | 1991-1995 | <18 | Not Reported | Monthly Min, Max and Mean Temperature | Historical Cohort | C | NR | NR | Dew point, Relative Humidity, Barometric Pressure and Wind Speed | Multiple Regression | No effect was seen with an average temperature |
| 23 | Witonsky,2018,USA(28) | 43729 | 2001-2008 | All age groups | ICD9-(493.00) | Weekly Mean Temperature | Ecologic | C | NR | NR | NO2,O3,PM2.5, SO2, precipitation, air pressure, humidity, tree pollen, grass pollen, and weed pollen. | Spearman Correlation | In pediatric patients, the multivariate coefficients for temperature and asthma related emergency department visits in the full year was –0.351 and in fall was–0.335 |
* Temperature variation between neighboring days (TVN)
?Not Reported
In order to further examine the geographical distribution and the characteristics of the area in which the studies were conducted, the Köppen-Geiger climate classification was used, which includes 5 climate zones (figure 2). Three of the studies had been done in the equatorial region17, 21, 22. There were no studies from the arid and polar regions. The remaining studies were from the warm-temperate4, 12, 16, 19, 20, 23-26, 28-35 and snow regions18, 27, 36.
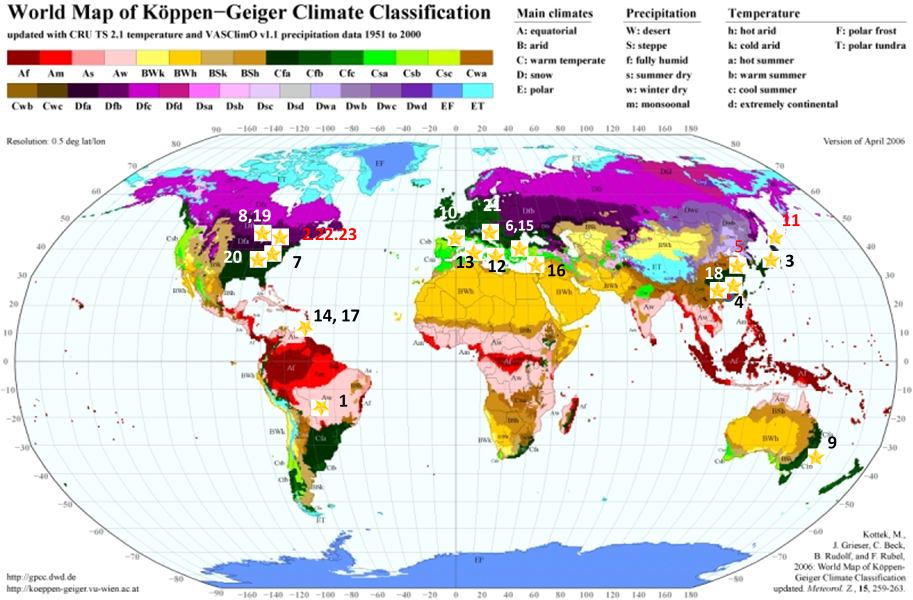
Figure 2: Distribution of studies across five Köppen Geiger climate zones (A–E). Study numbers on the map are defined in Table 1.
The studies included between one to nineteen years data. Studies had used different variables for measuring ambient temperature. Daily minimum, maximum and mean temperatures were the most common variables used in 16 studies4, 12, 16-19, 21, 22, 24, 25, 28, 29, 31, 32, 34-36 followed by monthly minimum, maximum and mean temperature in 5 studies20, 23, 26, 30, 33 and one article used hourly meteorological data27.
Different definitions had been used to define the outcome in different articles. Although all studies were conducted after the release of the Ninth Revision of the International Classification of Diseases, only 8 studies had used ICD94, 16, 25, 27, 28, 30, 31, 34. Five studies had used code 493.00 and 3 studies had used code 493.00 to 493.99. Also, two studies had used ICD10- (J45) as the outcome variable17, 35. The rest of the studies measured outcome based on physicians' assessment, the presence of asthma-related symptoms and the administration of nebulized bronchodilators. Two studies did not report how the asthmatic attack was diagnosed26, 29.
The results of 10 studies showed that the number of cases of asthma exacerbation was higher in boys than girls, while two studies reported a higher number of cases of asthma in girls than boys4, 27, and one study reported an equal number of cases36.
Studies had considered different lag periods between exposure and outcome, which varied from 0 to 60 days, but 8 studies did not include lag time19-21, 23, 24, 26-28. In many studies, the temperature was not the only risk factor considered; and demographic factors such as sex, race and meteorological factors such as barometric pressure, relative humidity, wind speed, rainfall and air pollutants, such as PM10, PM2.5, O3, NOX, were also examined. But these variables were different in different studies.
Fourteen studies were simple ecological studies, and two were case-crossover studies27, 34. Two studies had used the time-series method24, 31. Seven studies had used correlation coefficients16, 17, 19, 20, 24, 28, 29 and four studies had used relative risks to examine the relation between air temperature and asthma exacerbations12, 25, 27, 31.
Fourteen studies had reported a relation between cold temperature and recurrence of asthma and showed as the temperature dropped, the number of asthma attacks or the number of visits to hospitals for asthma increased in children12, 16, 17, 19, 20, 24, 28-35. Nine papers observed a relation between hot weather and asthma attacks4, 18, 21, 22, 25, 31, 32, 35, 36, and 3 studies reported a relation between temperature differences and asthma attacks13, 18, 34. Two studies did not show any relation between asthma attacks and temperature variables26, 27.
Studies in Malta and Spain showed that the increase in the incidence of asthma in the 5-14 age group was associated with the school re-opening season, and with a two-week lag after the start of the school year, recurrence of asthma increased in this age group19, 20, 22, 30.
Among the papers reviewed, 11 papers had examined the effect of seasons on the recurrence of asthma in children. Based on the Köppen−Geiger Climate Classification 16 studies were conducted in a warm-temperate climate4, 12, 16, 19, 20, 23-26, 29-35. Three articles were from the equatorial region12, 25, 34 and three articles were from the snow region13, 18, 37. Study results were different, but mainly the highest frequency of asthma occurred in autumn and spring4, 16, 20, 22, 24, 26, 28, 30, 34-36.
According to the World Economic Situation and Prospects38, most studies (16 studies) had been conducted in developed countries; including Croatia, the US, Japan, Australia, Greece, Malta and Spain; and seven studies had been conducted in developing countries, including China, Trinidad and Tobago, Hong Kong, Israel and Brazil17, 19, 21-23, 31, 32, while no study had been conducted in less developed countries.
Discussion
Most of the studies showed that extreme ambient air temperature has a relation with the recurrence or hospitalization of children due to asthma. For example, in Tokyo, as temperature decreased12, and in New York, as temperature increased, the incidence of asthma attacks in children increased4. The average daily temperature in Tokyo is 11 °C, while in New York City during cold spells it is -15 °C4 and New York has colder winters in comparison to Tokyo. Probably children with asthma during the winter season and during the cold spell, because of medical orders, changed their behavior and were less likely to expose themselves to the cold environment or use a mask to prevent asthma attacks.
Cold and hot temperatures affect the respiratory system through different mechanisms. Warm weather may cause microorganisms, mites and cockroaches to grow in the interior of human dwellings, or warm air can cause increased air pollution such as an increase in ozone and PM10. This, maybe one of the factors associated with inflammation of the respiratory tract and the recurrence of asthma.
Studies have also shown that cold and dry air increases the risk of airway inflammation, reduces lung function and reduces lung capacity37, 39-41. Cold weather can decrease moisture in the mucosal membrane of the respiratory tract, predispose it to irritation by allergens, cause sensitivity to viral and bacterial infections and increase the risk of asthma attacks42.
Studies conducted in Japan and America reported a direct relation between temperature changes, one day before the recurrence of asthma in children18, 24, 26, 27, 29, 35, 36. But, children under 5 years of age were less likely to be affected by air temperature changes due to less contact with the outside and environmental triggers31, 34, 35.
However, the high recurrence rate of asthma in school age children can be due to temperature changes and the transition from summer to autumn and due to the easier transmission of respiratory diseases after school opens. Respiratory pathogens in these children affect the relation between air temperature and the recurrence of asthma. Students can transmit these respiratory diseases to other family members, and a recurrence of asthma may be seen in other age groups as well16, 20, 22, 30.
The reason for the difference in recurrence of asthma in different times of the year can be due to the effects of various climatic or demographic variables, air pollutants, viral infections, and indoor aeroallergens43. In spring, the increased incidence of asthma may be related to fungal spores and pollen grains, while in autumn it may be due to rapid changes in temperature44, 45.
Most of the studies used in this review were ecological studies and one of the limitations of these studies was the assumption that the level of exposure was equal throughout the population and in different social and economic classes; and as well as the amount of time spent outdoors, and the use of air conditioner, heater and humidifiers. Also, in these studies, the reference population of patients visiting the hospitals under investigation was not clear. Only two studies used postal codes to determine the patients' location of residence and excluded children who were not living in that area34, 36.
Another limitation was not using the same patient classification system in the studies, as only 10 studies used the International Classification of Diseases4, 16, 17, 25, 27, 30, 31, 34, 35. Other studies used physician's assessment, the presence of asthma symptoms, or a history of using asthma drugs; for diagnosing asthma attacks. Two studies did not report the criteria used for diagnosing asthma attacks26, 29.
Conclusion
Ambient air temperature is probably related to the recurrence and hospitalization of child asthmatic patients. The results of some studies have shown that extremely hot and cold temperatures both increase the incidence of asthma in children. However, hot and cold temperature cause asthma attacks through different mechanisms.
References
- Khamutian R, Najafi F, Soltanian M, et al. The association between air pollution and weather conditions with increase in the number of admissions of asthmatic patients in emergency wards: A case study in Kermanshah. Medical Journal of the Islamic Republic of Iran. 2015; 29(1).
- World Health Organization. Asthma Fact sheet No 307. 2013. http://www.who.int/mediacentre/factsheets/fs307/en/ (Updated April 2017).
- Brzezi?ska-Paw?owska OE, Rydzewska AD, ?uczy?ska M, et al. Environmental factors affecting seasonality of ambulance emergency service visits for exacerbations of asthma and COPD. Journal of Asthma. 2016; 53(2): 139-45.
- Fitzgerald EF, Pantea C, Lin S. Cold Spells and the Risk of Hospitalization for Asthma: New York, USA 1991–2006. Lung. 2014; 192(6): 947-54.
- Dadbakhsh M, Khanjani N, Bahrampour A, et al. Death from respiratory diseases and temperature in Shiraz, Iran (2006–2011). Int J Biometeorol. 2017; 61(2): 239-46.
- Khanjani N, Bahrampour A. Temperature and cardiovascular and respiratory mortality in desert climate. A case study of Kerman, Iran. Iranian journal of environmental health science & engineering. 2013; 10(1): 11.
- IPCC.Climate Change 2014 Synthesis Report Summary for Policymakers. https://www.ipcc.ch/report/ar5/syr/ (Updated july 2017).
- IPCC. Summary for Policymakers. In: Stocker TF, Qin D, Plattner G-K, Tignor M, Allen SK, Boschung J, et al., editors. Climate Change 2013: The Physical Science Basis Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, United Kingdom and New York, NY, USA: Cambridge University Press; 2013. p. 1–30.
- Buckley JP, Richardson DB. Seasonal modification of the association between temperature and adult emergency department visits for asthma: A case-crossover study. Environmental Health: A Global Access Science Source. 2012; 11(1).
- Picado C. Barcelona's asthma epidemics: clinical aspects and intriguing findings. Thorax. 1992; 47(3): 197-200.
- Silverstein M, Mair Je Fau - Katusic SK, Katusic Sk Fau - Wollan PC, et al. School attendance and school performance: a population-based study of children. (0022-3476 (Print)).
- Hashimoto M, Fukuda T, Shimizu T, et al. Influence of climate factors on emergency visits for childhood asthma attack. Pediatrics International. 2004; 46(1): 48-52.
- Abe T, Tokuda Y, Ohde S, et al. The relationship of short-term air pollution and weather to ED visits for asthma in Japan. The American Journal of Emergency Medicine. 2009; 27(2): 153-9.
- Anderson GB, Dominici F, Wang Y, et al. Heat-related Emergency Hospitalizations for Respiratory Diseases in the Medicare Population. Am J Respir Crit Care Med. 2013; 187(10): 1098-103.
- Xu Z, Crooks JL, Davies JM, et al. The association between ambient temperature and childhood asthma: a systematic review. International journal of biometeorology. 2017; 1-11.
- Altzibar JM, Tamayo-Uria I, De Castro V, et al. Epidemiology of asthma exacerbations and their relation with environmental factors in the Basque Country. Clinical and experimental allergy : journal of the British Society for Allergy and Clinical Immunology. 2015; 45(6): 1099-108.
- de Souza A, Santos DAS, Lima APS, et al. Impact of changes in meteorological and hospitalizations for asthma. Espacios. 2015; 36(11).
- Ehara A, Takasaki H, Takeda Y, et al. Are high barometric pressure, low humidity and diurnal change of temperature related to the onset of asthmatic symptoms? Pediatrics international : official journal of the Japan Pediatric Society. 2000; 42(3): 272-4.
- Garty BZ, Kosman E, Ganor E, et al. Emergency Room Visits of Asthmatic Children, Relation to Air Pollution, Weather, and Airborne Allergens. Annals of Allergy, Asthma & Immunology. 1998; 81(6): 563-70.
- Grech V, Balzan M, Asciak RP, et al. Seasonal variations in hospital admissions for asthma in Malta. The Journal of asthma : official journal of the Association for the Care of Asthma. 2002; 39(3): 263-8.
- Ivey MA, Simeon DT, Juman S, et al. Associations between climate variables and asthma visits to accident and emergency facilities in Trinidad, West Indies. Allergology International. 2001; 50(1): 29-33.
- Ivey MA, Simeon DT, Monteil MA. Climatic variables are associated with seasonal acute asthma admissions to accident and emergency room facilities in Trinidad, West Indies. Clinical and experimental allergy : journal of the British Society for Allergy and Clinical Immunology. 2003; 33(11): 1526-30.
- Liu XM, Zhou XB, Shuang L, et al. Relations between meteorological factors and asthma in children from Qingdao city. Journal of Clinical Rehabilitative Tissue Engineering Research. 2007; 11(16): 3181-3.
- Nastos PT, Paliatsos AG, Priftis KN, et al. The effect of weather types on the frequency of childhood asthma admissions in Athens, Greece. Fresenius Environmental Bulletin. 2006; 15(8 B): 936-42.
- O’Lenick CR, Winquist A, Chang HH, et al. Evaluation of individual and area-level factors as modifiers of the association between warm-season temperature and pediatric asthma morbidity in Atlanta, GA. Environmental Research. 2017; 156: 132-44.
- Palusci VJ, Mustalish EK, Fine J, et al. Does the weather trigger pediatric asthma emergency department visits? Ambulatory Child Health. 1998; 3(4): 357-63.
- Wasilevich EA, Rabito F, Lefante J, et al. Short-term outdoor temperature change and emergency department visits for asthma among children: a case-crossover study. American journal of epidemiology. 2012; 176 Suppl 7: S123-30.
- Witonsky J, Abraham R, Toh J, et al. The association of environmental, meteorological, and pollen count variables with asthma-related emergency department visits and hospitalizations in the Bronx. Journal of Asthma. 2018.
- Zaninovi? K, Raos M. The influence of meteorological parameters on asthmatic attacks in children. Hrvatski Meteoroloski Casopis. 2001; (37): 89-94.
- Hervas D, Utrera JF, Hervas-Masip J, et al. Can meteorological factors forecast asthma exacerbation in a paediatric population? Allergologia et immunopathologia. 2015; 43(1): 32-6.
- Lam HCY, Li AM, Chan EYY, et al. The short-term association between asthma hospitalisations, ambient temperature, other meteorological factors and air pollutants in Hong Kong: A time-series study. Thorax. 2016; 71(12): 1097-109.
- Li K, Ni H, Yang Z, et al. Effects of temperature variation between neighbouring days on daily hospital visits for childhood asthma: a time-series analysis. Public Health. 2016; 136: 133-40.
- Nastos PT, Paliatsos AG, Papadopoulos M, et al. The effect of weather variability on pediatric asthma admissions in Athens, Greece. The Journal of asthma : official journal of the Association for the Care of Asthma. 2008; 45(1): 59-65.
- Soneja S, Jiang C, Fisher J, et al. Exposure to extreme heat and precipitation events associated with increased risk of hospitalization for asthma in Maryland, U.S.A. Environmental Health: A Global Access Science Source. 2016; 15(1).
- Xu ZW, Huang CR, Hu WB, et al. Extreme temperatures and emergency department admissions for childhood asthma in Brisbane, Australia. Occupational and Environmental Medicine. 2013; 70(10): 730-5.
- Mireku N, Wang Y, Ager J, et al. Changes in weather and the effects on pediatric asthma exacerbations. Annals of Allergy, Asthma & Immunology. 2009; 103(3): 220-4.
- Bartoli ML, Vagaggini B, Malagrinò L, et al. Baseline airway inflammation may be a determinant of the response to ozone exposure in asthmatic patients. Inhal Toxicol. 2013; 25(3): 127-33.
- World Economic Situation and Prospects 2016. http://www.un.org/en/development/desa/policy/wesp/wesp_current/2014wesp_country_classification.pdf. United Nations publication.
- Bartoli ML, Vagaggini B, Malagrinò L, et al. Baseline airway inflammation may be a determinant of ozone response in asthmatic patients. Eur Respiratory Soc; 2012.
- Scannell C, Chen L, Aris RM, et al. Greater ozone-induced inflammatory responses in subjects with asthma. Am J Respir Crit Care Med. 1996; 154(1): 24-9.
- Weinmayr G, Romeo E, De Sario M, et al. Short-term effects of PM10 and NO2 on respiratory health among children with asthma or asthma-like symptoms: a systematic review and meta-analysis. Environ Health Perspect. 2010; 118(4): 449.
- Koskela H, Tukiainen H, Kononoff A, et al. Effect of whole-body exposure to cold and wind on lung function in asthmatic patients. Chest. 1994; 105(6): 1728-31.
- Escamilla-Nuñez MC, Barraza-Villarreal A, Hernandez-Cadena L, et al. Traffic-related air pollution and respiratory symptoms among asthmatic children, resident in Mexico City: the EVA cohort study. Respiratory Research. 2008; 9(1): 74.
- Johnston NW, Johnston SL, Duncan JM, et al. The September epidemic of asthma exacerbations in children: a search for etiology. Journal of Allergy and Clinical Immunology. 2005; 115(1): 132-8.
- Berktas B, Bircan A. Effects of atmospheric sulphur dioxide and particulate matter concentrations on emergency room admissions due to asthma in Ankara. Tuberk Toraks. 2003; 51(3): 231-8.
