Ventilator-Associated Pneumonia and In-Hospital Mortality: Which Risk Factors may predict In-Hospital Mortality in Such Patients?
Alizamin Sadigov*, Irada Mamedova, Kamran Mammmadov
Pulmonary Medicine Department, Azerbaijan Medical University, Baku
Abstract
Background: Ventilator-associated pneumonia (VAP) remains a common case of intensive care unite (Ä°CU) and hospital morbidity and mortality despite advances in diagnostic techniques and manegment. One of most important point for such patients is identification of predictors for mortality in term for futher their modification and reduction of mortality rate.
Objective: We aimed to determine the most important risk factors for short-term mortality in patients with VAP in mechanically ventilated patients.
Methods: This retrospective study was carried out from February 2014 to January 2019. One hundred twenty one adults patients with VAP maintained on mechanical ventilation for more than 48 h in our ICU department were enrolled in the study. VAP was diagnosed as new persistent pulmonary infiltrates on chest radiographs and a least two of following: (1) Fever of ≥38.3C (2) leukocytosis of ≥ 12.000/mm3 and (3) purulent tracheobronchial secretions. Endotracheal aspirate (ETA) samples and blood samples of suspected case were collected and processed as per standard protocols.
Results: The primary underlying diagnosis and comorbidities were acute exacerbation of chronic obstructive pulmonary disease (AECOPD) in 42 patients, congestive heart failure in 32, neurological disease in 28, and renal disease in 19 patients. Gram-negative agents were the major of finding pathogen (Acinotebacter baumannii accounting for 37.1 %). This infection in 43 case (95.5%) was multi-dying resistant (MDR) pathogen and associated with significantly higher length of ventilation (LOV) and the length of ICU stay (LOSicu) (p=0.01 respectively). Severe sepsis/septic shock, acute respiratory distress syndrome (ARDS), malnutrition, pulmonary complications such as pleural effusions and bilateral, multi- lobar lung infiltrates were most common findings in VAP patients which were associated with higher mortality (p<0.01).Acinotebacter baumannii MDR pathogens was associated with higher mortality rate compare with other MDR pathogens (p<0.01).
Conclusion: Ventilator-associated pneumonia is a serious ICU complication that is associated with increased in hospital mortality.In patients with VAP malnutrition ,severe sepsis/septic shock, ARDS, MDR Acinotebacter baumannii infection ,bilateral pulmonary infiltrates ,and underlying chronic obstructive pulmonary disease(COPD) are associated with increased risk in-hospital mortality in such patients. Identification of risk factor for in hospital mortality in such patents is important in term on further their modification and reduction of mortality rate.
Introduction
Patients in ICU are usually at high risk of mortality not only from their illness but also from secondary complication such as nosocomial infection. Nosocomial pneumonia a common ICU infection affects 27% of all critically ill patients where 86% of it is associated with mechanical ventilation1.
According to the infections disease society of America/American Thoracic society (IDSA/ATS) guidelines (2016), hospital-acquired/nosocomial pneumonia (HAP) is pneumonia that occurs 48 h or more after admission and did not appear to be intubating at time of admission. On the other hand VAP is a type of HAP that develops more than 48-72 h after endotracheal intubations2. Moreover, VAP occurs in 28% of patient who receive mechanical ventilation where its rate of occurrence varies with the duration of mechanical ventilation. The diagnostic clinical triad of VAP consist of pulmonary infections signs including fever, purulent secretions and leukocytosis together with bacteriologic evidence of pulmonary infections and radiological suggestion of pulmonary infections3.
The mortality rate for VAP ranges between 27 and 76% Pseudomonas and Acinetobacter pneumonia is associated with higher mortality rates than those associated with other organisms studies have consistently shown the a delay in starting appropriate and adequately dosed antibiotics therapy increased the mortality rate4. Furthermore, VAP has been associated with prolonged ICU length of stay (LOCicu) and higher costs for medical care since ICUs incur and important part of hospital expenses. Therefore, prediction of risk factors and prevention of VAP could reduce the care utilized dosing hospitalization and decrease resource utilization and subsequent expenses5. Furthermore, very few studies have evaluated risk factors and markers of in hospital mortality in VAP patients in ICU residents6,7,8.
The aim of this study was the retrospective analysis of patients in ICU whom develops VAP to evaluate clinical features and predictors of mortality in this setting.
Patients and methods
This was a retrospective study conducted at ICU department of Therapeutic and Education clinic of Medical university Azerbaijan, Baku city, occurring time period from February 2014 to January 2019. One hundred twenty one adult (18 yrs) patients with VAP were enrolled in the study Inclusion criteria: hospitalized, intubated, and mechanically ventilated patients whom pneumonia was developed more than 48 h after intubation.
Pneumonia was diagnosed as VAP when it occurs after 48 h of endobroncial intubation and mechanical ventilated. The criteria of diagnosis are new persistent pulmonary infiltrates appearing on chest radiographs and a least two of following: (1) fewer of ≥38° C (2) leukocytosis of ≥ 12.000/mm3 and (3) purulent tracheobronchial secretions. In case of clinically suspected pneumonia endobronchial aspirate and blood culture (in case of fewer ≥38° C) was sent for microbiology and diagnosis of VAP was established with positive quantitative culture (cut off point ≥106 CFU/ml). It was mainly the number (cut off point-above this number) of colony-forming units in endobronchial aspirate. To analyze the predisposing factors and in hospital mortality the following variables were evaluated: age , gender, other comorbidities (COPD on admission), the clinical diagnosis at time of hospitalization, length of ICU stay length of ventilation and development of complications. Patients were excluded from the study if one of the following criteria were applied radiographic evidence of preexisting infiltrates or criteria for hospital-acquired pneumonia9.
All comorbidities were defined as previously described10. Chronic kidney disease (CKD) stage was defined according to current guidelines (2012 KDIGO Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease,11). Diagnosis of malnutrition was based on the presence of one more of the following criteria: body mass index less than <21 kg/m2; serum albumin concentrations <3.5 g/l12,13. The BMI less than 21kg/m2 was basic for identification of malnutrition. Septic shock was defined as bacteraemia and hypotension requiring use of vasopressors14. The severe pneumonia as known is defined with septic shock requiring use of vasopressors and need to mechanical ventilation. In out study considering that all our patients were in mechanical ventilation ,all patients with VAP were severe pneumonia. A patient was considered to have a MDR pathogen if one of the following pathogens was extended spectrum beta lactamase (ESBL) –producing or carbapenem-resistant Enterobacteriaceae, methicillin-resistant staphylococcus aureus (MRSA) stenotrophomonas maltophilia or Acinetobacter baumannii. MDR pathogens were defined by identification one pathogenic agent resistance to three different class antibiotics. For the remaining case, MDR was defined as isolation of bacteria strain non- susceptible to at least one agent in three or more antimicrobial categories15.
Study endpoints and statistical analysis
The study endpoints were the assessment in hospital mortality. To identify risk factors associated with in hospital mortality, we performed univariable and multivariable analysis. To detect significant differences between groups we used the chi square test or Fisher’s exact test for categorical variables and the two tailed test or Mann-Whitney test for continuous variables when appropriate continuous variables were reported as medians with interquartile ranges (IQR): numbers and percentages were reported for categorical variables. Baseline variables (recorded at pneumonia onset) were analyzed in the univariable analysis and induced in the multivariable analysis to identify of in hospital mortality. Statistical significance was established at ≤0.05. All reported p values are two-tailed.
Result
Overall 121 patients with VAP were analyzed. In the investigated period the overall incidence rates of VAP was 30.5% (121 of 396 intubated patients). It suggested that the incidence and prevalence of VAP in mechanically ventilated patients was common. Table 1 describes baseline characteristics of our study population.
Table 1. Baseline characteristic of patients with VAP and univariable analysis comparing survivors and non-survivors
|
|
Overall N=121(%) |
Survivors N=69(%) |
Non-Survivors N=52(%) |
P value |
|
Males |
52/121(42.9) |
29/69(42.0) |
23/52(44.2) |
0.42 |
|
Females |
69/121(57.1) |
38/69(55.1) |
31/52(59.6) |
0.29 |
|
Age, median years |
64(52-78) |
54(52-69) |
70(62-78) |
0.01 |
|
Prior antibiotic therapy (last 90 days) |
78/121(64.4) |
42/69(60.9) |
36/52(69.2) |
0,21 |
|
Neurological disease |
28/121(23.1) |
7/69(10.1) |
22/52(42.3) |
0.005 |
|
Intracascular device (venous catheters) |
19/121(15.7) |
5/69(7.2) |
14/52(26.9) |
0.01 |
|
Chronic heart failure |
32/121(26.4) |
13/69(18.8) |
19/52(36.5) |
0.05 |
|
Renal disease |
19/121(15/7) |
4/69(5.8) |
15/52(28.8) |
0.001 |
|
COPD |
42/121(34.7) |
15/69(21.7) |
27/52(51.9) |
0.007 |
|
Haemodialysis |
14/121(11.5) |
4/69(5.8) |
10/52(19.2) |
0.01 |
|
Malnutrition |
36/121(29.7) |
10/69(14.5) |
26/52(51.9) |
0.001 |
|
Diabetes |
32/121(26.4) |
15/69(21.7) |
17/52(32.7) |
0.09 |
|
Pleural effusion |
53/121(43.8) |
16/69(23.1) |
38/52(73.1) |
0.001 |
|
Bilateral pneumonia |
63/121(52.1) |
22/69(31.8) |
41/59(78.8) |
0.007 |
|
Multi-lobar pneumonia |
89/121(73.5) |
40/69(57.9) |
49/52(94.2) |
0.01 |
|
Increased CRP(>5mg/l) |
111/121(91.7) |
62/69(89.8) |
49/52(94.2) |
0.28 |
|
PaO2/FiO2 ratio <_250 |
32/121(264) |
8/69(11.5) |
24/52()46.2 |
0.005 |
|
NIV before intubation |
58/121(47.9) |
23/69(33.3) |
35/52(67.3) |
0.01 |
|
Severe sepsis/Septic shock |
21/121(17.4) |
5(7.2) |
16/52(30.7) |
0.001 |
|
ARDS |
18/121(14.8) |
3/69(3.5) |
15/52(28.8) |
0.001 |
|
MDR pathogens |
82/121(67.8) |
44/69(63.7) |
38/52(73.0) |
0/09 |
|
Acinotebacter baumannii |
39/121(32.2) |
13/69(18.8) |
26/52(50.0) |
0/01 |
|
Non-Acinotebacter baumannii MDR pathogens |
43/121()35.5 |
24.69(34.8) |
19/52(36.5) |
0.24 |
|
Hospitalization before ICU admission |
59/121(48.7) |
33/69(47.8) |
26/52(50.0) |
0.31 |
COPD-chronic obstructive pulmonary disease; CRP- c-reactive protein; NIV- non-invasive ventilation; MDR- multi drug resistant; ARDS-acute respiratory distress syndrome.
Overall, the majority of patients (64.4%) received antibiotics in the previous 90 days (for any indications) and have evaluated multi -drug -resistant (MDR) pathogens (67.8%). However, both either prior antibiotic therapy and association with MDR pathogens don’t increase the hospital mortality in VAP patients (p=0.21, 0.19; respectively).Intravascular devices(central venous catheter such as subclavicular in patients receiving haemodialysis) were associated with increased risk of in-hospital mortality in patients with VAP.
Chronic heart failure (26.4%), COPD (34.7%), severe renal disease (15.7%, stage 4 and stage 5 chronic kidney disease with glomerular filtration rate between 15-30 ml/min and <15ml/min), malnutrition (29.7%) and neurological disorders (23.1%) were the most common underlying disease. On chest radiograph a plural effusion, bilateral pneumonia and multi-lobar pulmonary infection were common findings among non-survivors VAP patients compare to survivors VAP patients (p=0.001, 0.007, 0.01; respectively).
The incidence of severe sepsis/septic shock and ARDS at the time of intubation were higher among non- survivors VAP patients compared to survivors VAP patients (p<0.001, =0.001; respectively).
The presence of PaO2/FiO2 ratio ≤250 (the ratio of partial pressure of oxygen in the arterial blood to fractional concentration of oxygen in intubated patients) in patients significantly was associated with increased mortality (p=0.005). Although in- hospital or home use of non-invasive ventilation markedly associated with increased mortality rate in VAP patients (p=0.01).
Table 2. Pathogens isolated among in 94 patents with culture-positive VAP
|
Etiologies |
Overall n=94(%) |
Survivors n= 50(%) |
Non-Survivors n= 44(%) |
P value |
|
Acinotebacter baumannii |
39/94 (41.4) |
13/50(26.0) |
26/44(59.1) |
0.01 |
|
Pseduomanas aerigunosa |
30/94(31.9) |
14/50(28.0) |
16/44(36.3) |
0.12 |
|
MRSA |
12/94(12.8) |
7/50(14.0) |
5/44(11.4) |
0.18 |
|
Eserichia coli |
7/94(7.4) |
3/50(6.0) |
4/44(9.0) |
0.21 |
|
Klebsiella pneumonia |
6/94(6.3) |
4/50(8.0) |
2/44(4.5) |
0.16 |
|
MDR pathogens: Acinotebacter baumanni Pseudomonas aeruginosa
MRSA
Eschericia coli
Klebsiella pneumonia |
82/94(87.2)
37/39(92.3)
21/30(70.0)
10/12(83.3)
4/7(57.1)
3/6(50.0)
|
44/50(87.2)
10/39(25.6)
12/30(40.0)
5/12(41.6)
2/7(28.6)
2/6(33.3) |
38/44(86.4)
27/39(69.2)
9/30(30.0)
5/12(41.6)
2/7(28.6)
1/6(16.7) |
0.22
0.01
0.11
0.95
0.84
NS |
MRSA methicillin-resistant staphylococcus aureus; MDR multi-drug –resistant;NS-non-significant
Acinotebacter baumannii was the most commonly isolated pathogens (41.4% of case), followed by Pseudomonas aeruginosa (31.9%). Among 94 patients with etiological diagnosis, a MDR pathogens was identify 87% of cases. However, univariable analysis show that just Acinotebacter baumannii infection has increased the in hospital mortality rate in VAP patients (p=0.01; in non-survival patients with VAP the incidence of Acinotebacter baumanniiisolation was significantly higher compared to survival patients with VAP) . Other MDR pathogens were not associated with increased mortality among VAP patients (p=0.22). Multivariable analysis showed that malnutrition (serum albumin level≤ 3.5 g/l OR 8,1; 95% Cl 2,9-4.2 p<0.001), bilateral pneumonia (OR 4.2; 95%Cl 1,1-10.4 p=0.005) MDR Acinotebacter baumannii infection (3.4; Cl 95% 1.2-7.6, p=0.01).
COPD (OR 3.6 95% Cl 1.4-8.4 P=0.007) Severe sepsis\septic shock (OR 8.7; 95% Cl 2.9-26.8, p<0.001) and PaO2 FiO2 ratio ≤250 OR 7.9; 95% Cl 2.6-24.2 p=0.001) were independency associated with in hospital mortality (table 3).
Table 3. Multivariate analysis of in hospital mortality in VAP patients
|
Variables |
OR |
95%Cl |
P |
|
Malnutrition |
8.1 |
2.9-21.9 |
0.001 |
|
Bilateral pneumonia |
4.2 |
1.1-10.4 |
0.007 |
|
MDR Acinotebacter baumannii infection |
3.4 |
1.2-7.6 |
0.01 |
|
COPD |
3.6 |
1.4-8.4 |
0.007 |
|
Severe sepsis/septic shock |
8.7 |
2.9-26.8 |
0.001 |
|
Pa2/FiO2≤250 |
7.9 |
2.6-24.2 |
0.001 |
The performance of severity of VAP significantly increased mortality rate in patients and by increasing the number of independent risk factors for in hospital mortality the incidence of death has been increased (Fig.1).
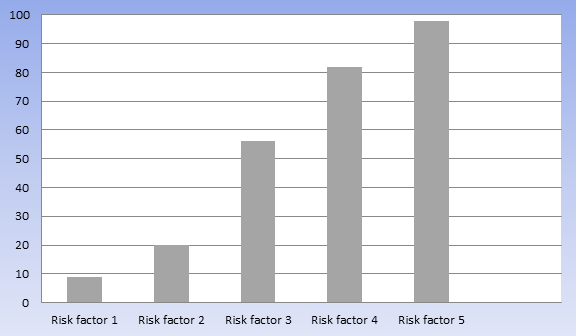
Fig.1 The relationship between combination risk factors and in hospital mortality rate in patient with VAP.
Combination of risk factors significantly increased the death rate among VAP patients and in the patients with five risk factors associated the mortality rate was 99%. Among all non-survivors patients the severe sepsis /septic shock was main risk factor leading to death of patients with VAP.
Discussion
ICU patients with VAP have specific risk factors associated with in hospital mortality and by retorpsective analiyis during five years period we identified baseline variables that are independently associated with death. Malnutrition, bilateral pneumonia, multi-drug-resistant Acinotebacter baumannii infection, severe sepsis/septic shock, COPD and PaP2/FiO2≤250 were independently associated risk factors for in- hospital mortality in VAP patients.
We have assessed 121 patients with VAP with high mortality rate (42.9%) and by baseline analysis of these patients we have found most important and independent risk factors for in hospital mortality finally compared with others VAP studies, we found that in this specific population, factors such as severe sepsis/septic shock and PaO2/FiO2 ≤ 250 play major role in predicting the risk of death. Our study has also some limitations. First it has been performed in patients on based retrospective analysis second the high frequency of MDR pathogens, especially Acinotebacter baumanii, in patients with etiological diagnosis may note be generalized to other ICU department with low prevalence of resistant bacteria.
Third we could not collect data baseline functional capacity of VAP patients just due o it was retrospective study and we thought that these data would be useful to predict risk of death.
We found that malnutrition is another major determinant of outcome. It has been previously show that the nutritional screening is a tool for identifying the most at the risk individuals16.
and that the of BMI more than 21 kg/m3 is associated with increased survival in pneumonia patients17. I suggest that low BMI was associated with worse outcomes and increased in-hospital mortality in VAP patients.
A diagnosis of COPD was present in 34.7% of the study population under this circumstance pneumonia can cause a rapid decline of vital signs and functions and also the occurrence of acute vascular complications18.
This it is not surprising the appearance of sign of severe impairment of lung function, hypotension and PaO2/FiO2 ratio ≤250 were strong predictors of death.
Among patients with an etiological diagnosis we found a high prevalence of MDR pathogens especially, multi-drug resistant Acinotebacter baumanni infection. This finding has been associated with increased mortality, primarily because of the higher risk of inappropriate initial antibiotic therapy [19]. However, in our study only Acinotobacter baumannii infection was independent risk factor associated with increased in hospital mortality VAP patients. Other MDR pathogens such as Psedumonas aureginosa, MRSA, Eserichia coli, and Klebsiella pneumnonia were not associated with increased risk of in- hospital mortality in VAP patients.
Our retrospective study provides to clinicians especially to ICU department physicians a tool to approach to identify the mortality risk of patients with VAP. Our study suggests that in VAP patients the presence of malnutrition, bilateral pulmonary infection, severe sepsis/septic shock, ARDS, multi-drug-resistant Acinotobacter baumannii pneumonia and chronic obstructive pulmonary disease are associated with poorly outcomes and significantly increased in hospital mortality. Thus, only the identification of patients with VAP with highest probability to die may help ICU clinicians pulmonologist, to decide on the best management of VAP.
References
- Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016 Sep 1; 63(5): e61-e111.
- Deborah J, Cook MD, Stephen D, et al. Incidence of and Risk factors for ventilator-associated pneumonia in critically ill patients. Ann Intern Med. 15 Sept 1998; 15(6): 433-46.
- Morehead RS, Pinto SJ.Ventilator-associated pneumoniua.Arch Intern Med. 2000; 160: 1926-36.
- Hogonner S, Vckay I, Piter D. Staffing level: a determination od late-onset ventilator-associated pneumonia. Crit Care. 2007; 11: R80.
- Langer M, Mosconi P, Cigada M, et al.Long-term respiratory support and risk of pneumonia in critically ill patients.Intensive Care Unit Group of Infection Control. Am rev Respir Dis. 1989; 140: 302-5.
- Tejerina E, Trutos-Vivar F, Restrepo M, et al.Incidence ,risk factors,and outcome of ventilator-associated pneumonia. J Crit Care. 2006; Mat21(4): 56-65.
- Chastre J, Fagon JY. Ventilator-associated pneumonia.Am J Respir Crit Care Med. 2002; 165(7): 867-903.
- Koller MH, Morrow LE, Neiderman MS, et al. Clinical characteristics and treatment ventilator-associated pneumonia. Chest. 2006; 129: 1210-28.
- Gudelines for the management of adults with hospital –acquired,ventilator-associated ,and healthcare –associated pneumonia. Am J Respir Crit Care Med. 2005; 171: 388-416.
- Esper AM, Moss M, Lewis CA, et al. The role of infection and comorbidity: factors that influence disparities in sepsis. Crit Care Med. 2006; 34: 2576-2582.
- Vincent JL, Rello J, Marshall J, et al.International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009; 302: 2323-2329.
- Bregeon F, Cias V, Carret V, et al.Is ventilator-associated pneumonia an independent risk factor for death?Anethesiology. 2001; 94: 554-560.
- Papazian I, Bregeon F, Thirion X, et al.Effect of ventilator –associated pneumonia on mortality and morbidity. Am J Respir Crit care Med. 1996; 54: 91-96.
- Hunter JD. Ventilator-associated pneumonia. BMJ. 2012; 344: e3325.
- Rodrigues DO, Cezario RC, Filho PP. Ventilator-associated pneumonia caused by multi-drug –resistant Pseudomonas aeruginosa vs other microorganisms at an adult clinical –surgical intensive care unit in a Brazilian University Hospital: Risk factors and outcomes. Int J Med Sci. 2009; 1: 432-7.
- Raynaud-Simon A, Revel-Felhom C, Hebuterne X. French Nutrition and Health Program. French Health High Authority.Clinical practice guidelines from the French Health High Authority: nutritional support strategy in protein-energy malnutrition in the elderly. Clin Nutr. 2011; 30: 312-29.
- Dhawan N, Pandya N, Khalili M, et al. Predictors of mortality for nursing home-acquired pneumonia: a systematic review. Biomed Res Int. 2015; 138: 1480-5.
- Kalanuria AA, Ziai W, Mirski M. Ventilator-associated pneumonia in ICU. Crit Care. 2014; 18(2): 208.https://doi.org/10.1186/cc13775.
