Pulmonary cryptococcocis in immunocompetent patient - a case report
C.A Hing1, A. Alaga1*, M.K Razul1
1Hospital Sultanah Bahiyah, Alor Setar, Malaysia
Abstract
Pulmonary crytococcosis is a rare infection in immunocompetent patients. It is caused by encapsulated yeast-like fungus Cryptococcus neoformans. A young healthy gentleman presented with 1 day history of dyspnoea and fever, with 2 weeks history of weight loss.
Clinical examination revealed left lung collapse. CT thorax done showed a mediastinal mass with left lung collapse. Tissue obtained from bronchoscopy confirmed presence of Cryptococcus neoformans. The left main bronchial mass was removed during rigid bronchoscopy to expand the left lung. He was given T fluconazole 400 mg OD for 6 months. He improved significantly after the removal of left bronchial mass.
Introduction
Pulmonary crytococcosis is a rare infection in immunocompetent patients.
Cryptococcal lung disease ranges from asymptomatic colonization or infection to severe pneumonia with respiratory failure. Clinical presentation of pulmonary cryptococcosis is highly variable and often is related to the immune status of the patient. In an epidemiological study of 1491 patients diagnosed with cryptococcosis between 1992 and 2000, a total of 58 (4%) presented with pulmonary disease and only 12 (0.8%) were not human immunodeficiency virus (HIV)-infected. There is no clear treatment algorithm available for this infection.
Case report
A 29 year old gentleman with no underlying medical illness presented with unintentional significant weight loss of 11 kilograms in 2 weeks. He complained of cough for 1 week and 1 day history of fever and dyspnoea with absence of neurological symptoms. There was no significant exposure to pigeons. He had never received any immunosuppressant in the past. On clinical examination, noted reduced chest expansion, reduced breath sound and dullness over left hemithorax with deviated trachea to the same side.
Human immunodeficiency virus was non reactive ( ELISA and Partial Agglunination). Immunoglobulin levels were normal. Cryptococcal Antigen was positive with titre 1:128. Random blood glucose was normal. Sputum acid fast bacilli was negative for 3 readings. Blood culture was negative.
A chest radiograph (Figure 1) showed left lung collapse.
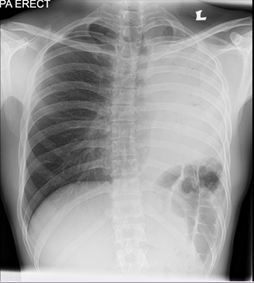
Figure 1.
CT Thorax (Figure 2) was performed on the same day showed a mediastinal mass with compression of the left main bronchus causing left lung collapse and mediastinal shift to the left.
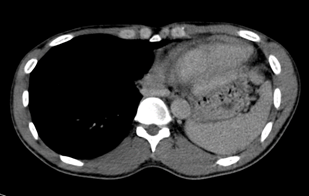
Figure 2.
The initial impression was lung malignancy. Differential diagnoses include teratoma or lymphoma.
Abbreviations: CI, confidence interval; COHb carboxyhemoglobin; WPS, waterpipe smoke
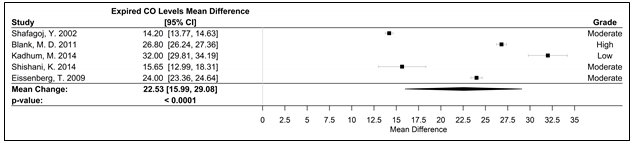
Figure 5. Forest plot of the mean difference of acute elevation in expired CO measured in ppm.
Abbreviations: CI, confidence interval, CO, carbon monoxide; ppm, parts per million; WPS, waterpipe smoke
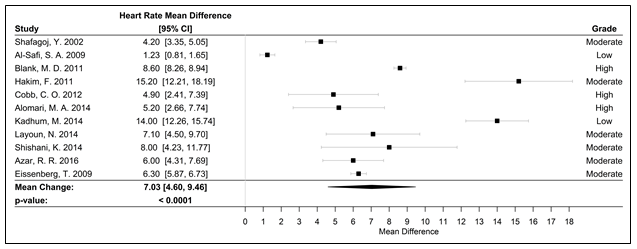
Figure 6. Forest plot of the mean difference of a WPS session and an acute elevation in HR measured in bpm
Abbreviations: bpm, beats per minute; HR, heart rate; WPS, water pipe smoke; CI, confidence interval
Flexible bronchoscopy was performed a week later and showed left main bronchial mass, a tissue sample was taken for histopathological examination. He was then scheduled for rigid bronchoscopy on the following week. The mass was able to be removed ( about 90% of total mass) during the procedure with serial dilatation of left main bronchus.
Chest radiograph post rigid bronchoscopy (Figure 4) showed left lung expansion.
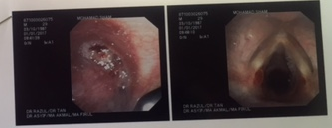
Figure 3. Left main bronchus (left) and vocal cord (right) from rigid bronchoscopy.
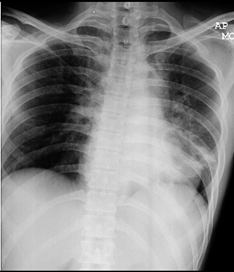
Figure 4. Chest radiograph post rigid bronchoscopy
The histopathological examination showed fairly large rounded microorganisms with cell walls that are highlighted by both periodic acid-schiff and Grocott methenamine silver stains resembling fungal bodies. Sputum and tissue culture showed Cryptoccocus neoformans.
The patient was started on intravenous Amphotericin B 40 mg daily but complicated with acute renal failure after 1 week of administration. He was then put on T Fluconazole 400 mg daily.
His appetite improved after the removal of intraluminal mass and he gained back 8 kilograms after 1 month.
He was assessed with rigid broncoschopy 1 month post treatment, we noted the previous left intraluminal mass has become smaller in size.
Chest radiograph (Figure 5) done, showed resolution of consolidative changes over left perihilar region with well expanded left lung 1 month after the bronchoscopy guided removal.
T Fluconazole 400 mg daily was continued for 6 months.
Flexible bronchoscopy was performed at the end of therapy, showed resolution of the intraluminal mass.
He was discharged well after 6 months of treatment. Repeated chest radiograph done was normal.
Discussion
Humans are likely to become infected with C. neoformans by inhaling the basidiospore form of the fungus or small, poorly encapsulated yeasts.
Isolated pulmonary cryptococcosis may be observed without specific therapy in asymptomatic immunocompetent hosts. However, considering that dissemination from a pulmonary infection can occur in patients with no immunologic defects, treatment of asymptomatic pulmonary cryptococcosis in immunocompetent hosts remains controversial.
There is no role for monitoring serum cryptococcal antigen titers to determine duration of therapy in either immunosuppressed or immunocompetent hosts Oral fluconazole is the main option for treatment of isolated pulmonary cryptococosis, the duration of treatment is not well defined
In the absence of diffuse pulmonary infiltrates or disseminated infection, suggested treatment consists of fluconazole (400 mg [6 mg/kg] orally daily ) for 6 to 12 months.
In our case study, the patient improved markedly after the removal of the intraluminal mass via rigid bronchoscopy. His chest radiograph normalized after 1 month of fluconazole. We extended his treatment to 6 months based on available literature reviews. Chest radiograph and flexible bronchoscopy were performed to follow up on treatment.
In immunocompromised patients, or those with severe disease, induction therapy with an amphotericin B preparation and flucytosine, followed by fluconazole as consolidation and maintenance therapy, is recommended.
The role of surgical resection for cure is reserved for patients who are not responding to medical therapy. In our case, he was subjected for removal of the endobronchial mass via rigid bronchoscopy as the initial histopathological examination taken from flexible bronchoscopy earlier on was still pending. The main purpose of the rigid bronchoscopy and removal of intraluminal mass was to relieve the left lung collapse.
Conclusion
Realizing that there is no clear treatment algorithm for isolated pulmonary crytococcosis in immunocompetent hosts, we would like to recommend for prospective studies to be done in the future to determine the duration of treatment with antifungal.
References
- John F Fisher, Paula A Valencia-Rey, William B Davis. Pulmonary Cryptococcosis in the Immunocompetent Patient—Many Questions, Some Answers, Open Forum Infectious Diseases. 1 May 2016; Volume 3, Issue 3: ofw167.
- Mirza S, Phelan M, Rimland D, et al.The changing epidemiology of cryptococcosis: an update from population-based surveillance in 2 large metropolitan areas, 1992–2000. Clin Infect Dis. 2003; 36: 789–94.
- Shirley RM, Baddley JW. Cryptococcal lung disease. Pub Med. May 2009; 15(3): 254-60.
