COVID-19 Pneumonia in Bilateral Lung Transplant Recipient: Case Report
Juan Pablo Reig Mezquida1*, Alilis Fontana Bellorín2, Alberto García Ortega3, Gabriel Anguera de Francisco1
1Lung Transplant Unit, Hospital Universitario la Fe, Valencia, Spain
2Department of Thoracic Surgery, Hospital Universitario la Fe, Valencia, Spain
3Department of Pulmonology, Hospital Universitario la Fe, Instituto de Investigación Sanitaria “La Fe”. Valencia, Spain
Abstract
The clinical course of Coronavirus disease 2019 (covid-19) in lung transplant recipients remains unknown. We present the fatal clinical course of a 63-year old double lung transplant recipient with severe Covid-19 pneumonia. She had stable graft function before Covid-19 infection. Despite all the supportive care and treatment graft injury progressed, causing patient death. Therefore, the prognosis in lung transplant recipients with Covid-19 infection is not optimistic.
Introduction
The current pandemic of Coronavirus Disease 2019 (COVID-19) has raised great alarm worldwide, but its impact on transplant patients is unknown, especially in lung transplant recipients. The immunosuppressive maintenance therapy leads to suppose that the course of this disease could be severe1. Spain has a National Transplant Organization which coordinates more than 100 lung transplants per year and gives support to transplant patients as at-risk population to COVID-19 infection. We report the fatal clinical course of a lung transplant recipient.
Case report
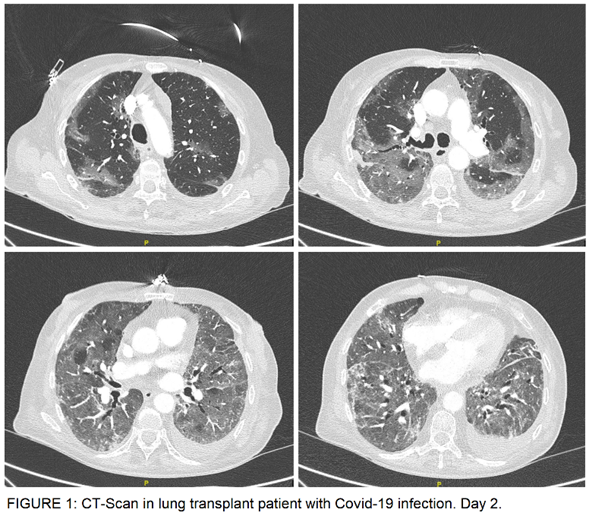
On March 31st, 2020, a 63-year-old woman, bilateral lung transplant carrier since January 2019, was admitted presenting severe bilateral Covid-19 pneumonia. Her previous lung capacity was normal and she received bilateral lung transplant due to end-stage emphysema. On admission, she was in poor general condition, diarrhea, fever, hypoxemia and tachypnea. Her laboratory results showed impaired renal function with creatinine of 2.45 mg/dL, lymphopenia of 0.06 x 103/µL (5%), C-reactive protein (CRP) of 110.3mg/L, Procalcitonin of 1.06 ng/mL, D-dimer of 2,571 ng/ml. At that moment, calcineurin inhibitor was replaced by low dose mTOR inhibitor Everolimus. Methylprednisolone was increased to 1mg / kg and meropenem was started. Prophylactic doses of enoxaparin, hydroxychloroquine (200mg daily) and Azithromycin 500mg/24h were prescribed. During the first 24h, the patient clinically improved, but on the third day her laboratory test showed a CRP of 203mg/L, the interleukin-6 (IL-6) levels increased to 308.9pg/mL, and D-dimer value raised to 60,479 ng/ml. The CT-scan reported an extensive ground-glass opacities affecting the middle lobe, lingula, and lower lobes, with consolidation areas and small left pleural effusion (Figure 1).
Everolimus blood levels were 1.8ng/mL. A single dose of anti-IL-6 antibody Tocilizumab was administered (400mg IV) and the patient remained respiratory stable and with sustained diuresis. On day 5 of admission, she developed a clinical deterioration, with pO2 of 46 mmHg, and was transferred to the Intensive Care Unit (ICU) where high-flow oxygen therapy was started (FiO2 of 100%, 60 L/min). At this moment, renal function continued worsening, associated with lower T-cell count, and procalcitonin raised to 9.92ng/mL. Immunosuppression was discontinued, Caspofungin was started and antibiotic therapy was changed to piperacillin-tazobactam. On day 7 mechanical ventilation was required due to physical exhaustion and lactate elevation. The renal function continued worsening and transaminases raised ten times normal values. Lymphopenia continued at values 0.08 x 103/µL (7%). Aspergillus niger was isolated from bronchial sample. Despite the support measures, the patient eventually died 9 days after admission due to multi-organ failure.
Discussion
The T-cell immune response to Covid-19 in lung transplant recipients remains unknown. It is expected to be suppressed due to the maintenance of immunosuppressive therapy usually with three drugs2. Some renal transplant recipients from China were described with good outcome3, and data from a single center experience in liver transplant recipients, suggested also similar outcomes to general population4. Recent data of solid organ recipients and Covid-19 infection have been published from a single-center, reporting a mortality rate of 27.8%5. Following the recommendations, immunosuppressive therapy was reduced to minimum dose and treated with Hydroxychloriquine, which has been proposed as a therapeutic option with promising results6. The change to mTOR inhibitor is performed in lung transplant patients with secondary renal impairment7, which has a depletive effect on interleukin IL-2R. IL2 overexpression has been also described in the cytokine release syndrome of severe Covid-19 pneumonia8, but the role mTOR inhibitors in Covid-19 remains unclear. The detection of Aspergillus in bronchial sample could be a secondary infection, first described in 30% of Covid-19 patients who required admission to the ICU1. The rapid course of infection in the patient we present, suggests that the outcome in lung-transplant population might be very poor. Triple therapy as maintenance immunosuppression, anatomical changes of the graft after transplant, and the lung as the target-organ of Sars-CoV2, could justify the worse clinical course of lung transplant recipients after Covid-19 pneumonia. Future pathological studies will be useful to clarify the differences between lung transplant recipients and immunocompromised patients.
Acknowledgement
Dr. Reig Mezquida, Dr. García Ortega and Dr. Anguera de Francisco treated the patient during hospitalization and contributed to the creation of the manuscript. Dr. Fontana Bellorín contributed to the creation and translation of the manuscript.
References
- Huang C, Wang X, Li L, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Feb; 15: 497-506.
- Scheffert JL, Raza K. Immunosuppression in lung Transplantation. Journal Thorac Dis. 2014 Aug; 6(8): 1039-53.
- Arpali E, Akyollu B, Yelken B, et al. Case Report: A kidney Transplant Patient with Mild COVID-19. Transplant infectious disease. 2020 Apr [Epub ahead of print].
- D'Antiga L. Coronaviruses and immunosuppressed patients. The facts during the third epidemic. Liver Transplantation. 2020 Mar [Epub ahead of print].
- Fernandez-Ruiz M, Andres A, Loinaz C, et al. COVID-19 in solid organ transplant recipients: a single-center cases series from Spain. American J of Transplantation. 2020 Apr [Epub ahead of print].
- Sarma P, Kaur H, Kumar H, et al. Virological and Clinical Cure in Covid-19 Patients Treated with Hydroxychloroquine: A Systematic Review and Meta-Analysis. Journal of Medical Virology. 2020 Apr [Epub ahead of print].
- Fine N, Sudhir K. Recent advances in Mammalian Target of Rapamycin Inhibitor Use in Heart and Lung Transplantation. Transplantation. 2016 Dec; 100(12): 2558-68.
- Chen G, Wu D, Guo W, et al. Clinica and immunological features of severe and moderate coronavirus disease 2019. The Journal olf Clinical investigation. 2020 Mar. [Epub ahead of print].
