A Social and Behavior Change Communication Framework for Addressing Delays to Appropriate TB Care and Treatment
Hala Jassim AlMossawi1, Colleen Longacre1, Yogan Pillay2, Neeraj Kak1*
1University Research Co, Chevy Chase, MD, USA
2National Department of Health, South Africa
Abstract
Social and behavior change (SBC) communication strategies and interventions have been used to successfully promote positive health behaviors and health outcomes, yet there is little evidence in the published literature on SBC frameworks for tuberculosis (TB) care and treatment. In this article, we outline a high-level generalized framework for the development, deployment, and evaluation of SBC communication strategies in high TB burden settings and how it could be employed to address TB treatment delays. The framework describes the contextual factors that will impact the design of a program, the spheres of influence, and details some of the outcomes to be achieved within each sphere that will lead to improved knowledge and substantive changes in behaviors at each prescribed level of the system. Improved design and delivery of SBC interventions can assist countries in meeting the Sustainable Development and Global End TB goals of reduced TB incidence, increased TB cure rates, reduced TB deaths, prevention of catastrophic out-of-pocket costs for TB care, and integration of health systems for patient-centered care.
Background
An effective tuberculosis (TB) control program requires early diagnosis and immediate initiation into treatment to reduce transmission. Delays in TB diagnosis and treatment can result in transmission of the infection to a greater number of people, as well as a more advanced disease at diagnosis and poorer response to treatment among the infected1. The Direct Observed Therapy-Short course (DOTS) strategy, while providing a critical framework for increasing TB treatment success, emphasizes passive case finding from persons who present themselves at health facilities. In a passive case finding approach, patients may delay seeking help or the health care system may delay in suspecting and/or investigating for TB. The weaknesses of this approach have led to a renewed focus on active case finding, and a shift in emphasis to approaches which empower front-line health care workers as well as patients and communities to play a more active role in recognizing their TB symptoms and seeking appropriate health care and TB treatment. Recent studies from high burden countries such as India have demonstrated that improving case finding methods may save 10 times more lives than the DOTS component2. However, TB treatment delays remain quite substantial, ranging from 30 – 366.5 days in many low- and middle-income countries3. Social and behavior change (SBC) communication interventions have increasingly been used to try and combat these TB treatment delays4,5.
SBC communication strategies and interventions have been used to successfully promote positive health behaviors and health outcomes in many health areas, including family planning, malaria, and HIV/AIDS6–9. While strategic frameworks for SBC communications exist for many of these health areas10–12, there is little evidence in the published literature on SBC frameworks for TB care and treatment13, although we do know that SBCC strategies are being employed to address TB in a wide variety of settings at both the patient and provider level4,5,14–16. In this article, we outline a high-level generalized framework for the development, deployment, and evaluation of SBC communication strategies in high TB burden settings and how it could be employed to address TB treatment delays. The framework describes the contextual factors that will impact the design of a program, the spheres of influence, and details some of the outcomes to be achieved within each sphere that will lead to improved knowledge and substantive changes in behaviors at each prescribed level of the system. Each of these processes are designed to contribute to a larger health system level outcome, in this case, sustainable reduction in TB incidence and increase in TB cure rates.
SBCC Framework to Accelerate the Response to TB
Our framework is guided by the theory of behavior change outlined in the Health Belief Model (HBM), one of the most widely applied theories of health behavior17,18. This model identifies six elements that contribute to predicting health behavior: risk susceptibility, risk severity, benefits to action, barriers to action, self-efficacy, and cues to action. Figure 1 outlines how each of these concepts can be leveraged for TB control through focused applications. As outlined below, communities need to understand their susceptibility to TB and how they can prevent getting it or transmitting it to others if they have it. This understanding needs to be with the community at large but also among healthcare workers. A major challenge faced by TB programs is that communities do not perceive the risk of getting TB and as a result influencing behavior to reduce the risk of transmission or contracting the disease remains a challenge. Also, communities as well as other healthcare workers need to understand the role of basic infection control, nutrition and sanitation that plays a role in increasing susceptibility to the disease. The key change agents for behavior change at community levels can include family as well as the immediate community, at facility levels it must include both service providers as well as specially assigned health education and counseling professionals. For program managers and policy makers, the change must be pushed by both community and special initiatives within the ministries of health and finance. The fundamentals to behavior change include targeted information as well as motivational pushes that could lead to acceptance of healthy behaviors.
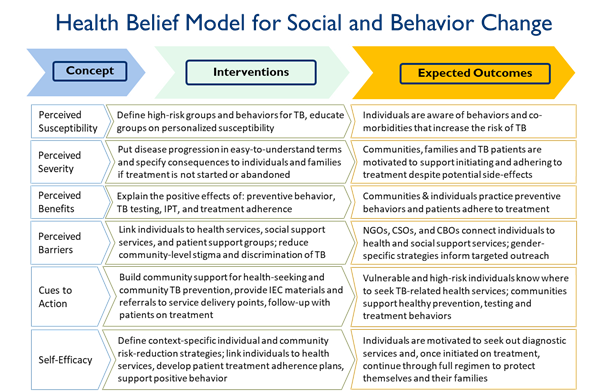
Figure 1: Key Approaches to SBCC Using the Health Belief Model
Context
Successful application of the HBM with sufficient acknowledgment of the influence of social, economic, or other environmental factors is critical19. The underlying environment in which a TB prevention, identification, and treatment program operates directly impacts the design, feasibility, and implementation of the program. The contextual factors that should be considered include: population size, disease burden and distribution, social constructs, cultural practices, economic environment, political environment, legal environment, and existing communication capacity at health systems and community levels. In addition to the various contextual factors that might impact the feasibility, acceptability, and sustainability of an SBC program for TB, an understanding of the fundamental barriers or challenges to effective programming must be considered.
Resources
In high TB burden countries, the responsibility of SBC should be shared by the leadership and should come from the National TB Programs (NTPs). NTPs need to engage various stakeholders in the design and execution of the SBC interventions. The inputs that must be evaluated and considered in the design and implementation of an SBC TB program will determine the quantity of fiscal and human resources to be mobilized, level of policy and strategy alignment, coordination with concurrent development programming, and existing policies determining implementation and evaluation needs. Prior to undertaking an SBC program targeting TB in a high burden setting, it is important to gain an understanding of available resources, how they have been allocated through a strategic plan or health plan, and the strengths and weaknesses of existing TB sector and communications policies and guidelines. Resources should be effectively distributed across the TB care pathway and comprehensively target health systems, provider, community and patient level behavioral factors which hinder timely TB diagnosis and successful treatment.
Spheres of Influence
To be successful, SBC interventions should be targeted to the appropriate sphere of influence. We have identified four spheres that programs may seek to target: the individual, the community, the health service delivery system, and the political and social environment (Figure 2). Understanding the various spheres of influence is critical to understanding and addressing the components which contribute to TB treatment delay20. Total delay is defined as the time between the onset of TB symptoms and the patient receiving appropriate TB treatment. Patient delay is defined as the time between the onset of symptoms and first contact with any type of health care service (formal or informal). Patient delay comprises two subgroups: 1) awareness delay, or the time between the onset of the symptoms and the recognition of those symptoms as a disease that needs healthcare assistance; and 2) access delay, or the time from the symptoms recognition to the first contact with a health care system. Health system delay is defined as the time between the first health seeking behavior and receiving TB treatment. Health system delay can also be divided into two sub-periods: 1) diagnostic delay, the time between a patient’s approach to the health system (public, private, healers) and the patient receiving the diagnosis of TB; and 2) treatment delay, the time between TB diagnosis and initiation of anti-TB drugs. This cascade of treatment delay plays out across spheres of influence that may be targeted by SBC interventions.
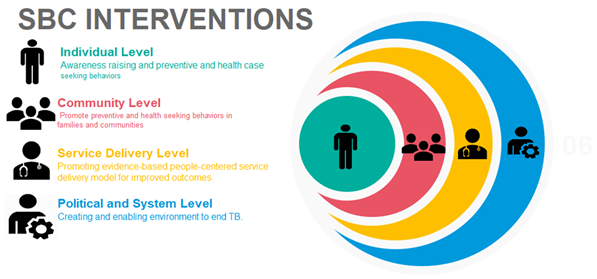
Figure 2: Using SBC to Target the Appropriate Spheres of Influence
Individual
The individual sphere of influence is becoming increasingly important in light of the World Health Organization (WHO)’s focus on more patient-centered approaches to TB care21. The intention of this effort is to ensure that those affected by TB remain a key focus in the design of TB control programs, and that health interventions are designed in a manner that respects the beliefs, values, needs and rights of those affected. The individual level is the primary source of patient-related TB delay. Factors contributing to primary patient delays are inherent to the patient and include demographic characteristics (age, gender, and marital status), individual health status, personal knowledge and attitude towards TB. In addition, negative personal and community attitudes towards TB patients which contribute to stigma and discrimination, influence primary patient delays. These factors influence patients’ recognition of their symptoms and their willingness or ability to seek care20. Patients’ low education and lack of knowledge of TB symptoms was attributed to 90% of TB patient delay in Tanzania (mean total delay of 185 days) with only 15% of the patients attending a health facility within 30 days of onset of symptoms22. A study from South Africa found that 41% of patients thought they would get better on their own and 13% cited they were too weak, scared or depressed to seek medical care23. Similar patient disempowerment was observed in a study from Russia24. Patient delay is also impacted by factors influencing access to health care centers such as geographic location, gender issues, costs and health seeking behavior patterns. Accessibility to a health facility was a significant predictor of delay in many countries20. Potential SBC interventions targeting this level could include: providing awareness to enhance people’s perceptions about TB as dangerous but curable disease; providing psychological support, counselling and health education, providing social support to TB patients and their households; building trusting relationships between the health care providers and people affected with TB; ensuring that health care providers comply with professional ethics and protect patients’ rights on confidentiality; using new technologies to support behavioral change (text messages, phone calls, digital medication monitors, etc.); and supporting roll out of various DOT modalities including access to Video Observed Therapy to ensure that patients with TB can choose the most suitable option that will allow them to successfully complete treatment.
Community
The community sphere of influence is very dependent on the implementation context and can include a variety of potential communication interventions. Interventions at this level are aimed at reaching appropriate audiences where they are most likely to uptake and retain health messaging to reduce stigma associated with TB infection and encourage appropriate care seeking behaviors. Potential SBC interventions targeting this level include: media campaigns, including radio, TV and SMS based messaging; print materials and posters throughout communities; social marketing; household-based awareness campaigns and provision of services; school and group-based campaigns; and community multi-sectoral strategic meetings.
Health Service Delivery System
This sphere includes the breadth of potential service providers, including health professionals delivering TB services, diagnostic testing staff, and community-based providers of DOTS. While most SBC efforts target national level policy and community/individual level behaviors, it is important to ensure that service delivery can meet increased individual and community demand with high quality and appropriate health care. The accessibility of appropriate TB diagnostics is an important factor in the proposed SBC model as increased demand should be met with increased supply of capacitated staff with adequate supplies to promptly test and refer TB patients. The service delivery system sphere of influence should be the primary target of health system delay. This delay is based on both patient and provider behaviors, providing prime opportunities for capacity building and strengthening to ensure patients that are presumptive for TB are appropriately tested for TB. The system delays are also reflective of political commitment. In many countries, senior policy makers from ministries of health, finance or planning do not understand the public health ramifications of poor or low investments on TB or other public health interventions resulting in continued high disease burdens. To influence the policy makers from these diverse constituencies, it is critical that advocacy and education efforts with data and other analytics are made on a regular basis. Part of this could include actual and societal costs with or without public health interventions. The National Department of Health in South Africa has established a TB Think Tank which is responsible for conducting data analytics and developing policy briefs25. The Think Tank has been successful influencing policy makers in allocating increased funding for the TB program since its inception. Another area that needs support of policy makers is that of engaging private sector in TB prevention and treatment initiation. This would include commitment of medical and nursing professional associations as well as seeking commitment of these organizations for policy makers by making sure that private providers are reimbursed for providing public health services to their patients26.
Treatment delay occurs when patients that test positive for a form of TB are not initiated on appropriate TB treatment. While there can be side effects and challenges to effective initiation on treatment, SBC programming and interventions can strategically encourage adherence to treatment regimens and provider capacity building to effectively link patient results with treatment initiation. Successful completion of TB treatment requires an effective partnership between the patient and health care professionals, and a harmony between the cultural context, the attitude of the patient, family support, and health literacy. Future health policies should address these issues to improve patients’ adherence to DOTS. Counseling of patients is important to optimize therapy, aid compliance, and to inform patients of any potential complications of therapy. Quality of counseling is determined by interpersonal communication skills of health care provider and whether or not the information delivered responds well to patient’s concerns, ideas, beliefs and knowledge gaps about TB and availability of TB services. Failure of completing treatment to some extent is explained by providers’ inability to adhere to evidence-based TB treatment guidelines which provide measures for effective management of TB drug-related side effects and patient counselling. Potential communication interventions targeting this level include: increasing the access to and familiarity with use of diagnostic testing; building IPC skills of providers through regular training and performance review; improving adherence to TB case management guidelines by providing job aids for various cadres of workers and regular skills building of health care workers and community based providers; improving availability of anti TB and auxiliary drugs for effective side effect management; supporting integration of TB/HIV, TB-diabetes and other relevant services, to ensure that patients’ needs are comprehensively addressed; and obtaining regular feedback on quality of care and understand the barriers which influence patient’s health seeking and adherence behavior through client satisfaction programming.
Social and Political Environment
This sphere includes large national resources and strategies that will influence policies and guidelines, advocacy, political will and multi-sectoral approaches to TB. Potential communication interventions targeting this level include: updating of National TB websites to provide updated information for various target audiences and build consensus around programmatic goals and innovations; updated policies and guidelines on TB prevention, screening and treatment specific to type of TB, and tailored to the needs of high risk and vulnerable groups (including HIV positive, migrants, prison inmates, mine workers, children and adolescent, pregnant women); media and policymaker advocacy; and coalition building through the formulation of multi-sectoral and multi-departmental coordination mechanisms with active involvement of people with TB experience and other civil society actors.
Outcomes for Evaluation
SBC interventions should be evaluated in terms of both progress outcomes and behavioral (health) outcomes. We have defined a set of potential outcomes for each sphere of influence to be targeted to track program progress, and well as population health outcomes that can be used to evaluate overall impact (Figure 3).
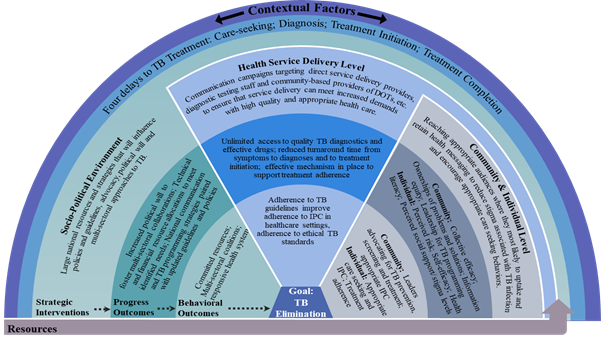
Figure 3: SBC Framework for TB
Individual
SBC interventions at the individual level should be aimed at improving individuals’ health literacy, including beliefs and attitudes about TB, perceived risk, perceived social support and stigma, and self-efficacy. Individual-level outcomes should be designed to evaluate the effect of SBC interventions on specific individual health seeking behaviors. These behaviors may include: early care seeking, adherence to treatment, adherence in appropriate infection prevention and control measures, and adherence to preventive measures for children and those at highest risk.
Community level
SBC interventions at the community level should be aimed at improving collective efficacy, ownership of problems and solutions, information equity, leadership for TB programming, and social capital. Community-level behavioral outcomes to be evaluated could include: advocacy for TB prevention, screening and treatment adherence by community leaders and local businesses; adherence to infection prevention and control standards to avoid TB transmission in families and communities; and participation in community-level services and coalition building.
Health service delivery system
SBC interventions at the service delivery level should be aimed at improving the availability of medicines and diagnostic resources, improving interpersonal communication techniques among providers, increasing integration of services, and improving support for patient treatment adherence. Positive provider-side behavioral outcomes could include: improved adherence to TB treatment guidelines, improved understanding and management of TB treatment side effects, increased quality of interpersonal counseling, greater respect for patients’ rights, and provision of more patient-friendly DOT services through various modalities.
Social and political environment
SBC interventions aimed at the political level should focus on creating and enabling an environment for TB control that fosters positive health seeking behavior by minimizing barriers to access to quality TB diagnosis and treatment and by mobilizing health and social systems and community resources for better adherence support. This includes: increased political will to improve access quality to TB services; increased resource allocation to meet identified needs; national strategies for social behavior change communications and TB programming paired with updated guidelines and policies; updated policies and guidelines for implementation throughout the system; increased institutional capacity building for effective SBC; and improved coordination and collaboration amongst sectors.
Implementation research
Research on people’s health seeking behaviors have the potential to make a tremendous impact on TB elimination efforts. Future implementation research should focus on: 1) how behaviors of both patients and providers affect TB-related care seeking, diagnosis, treatment success, and prevention; and 2) how other social, cultural, and environmental influences affect health seeking and treatment outcomes related to TB.
Conclusion
This SBC framework for TB is designed to help specific countries or programs to strategically employ available resources to reach target audiences through comprehensive SBC approaches to increase quality, equity, efficacy and sustainability of their TB programs. Improved design and delivery of SBC interventions will assist countries in meeting the Sustainable Development and Global End TB goals21,27 of reduced TB incidence, increased TB cure rates, reduced TB deaths, prevention of catastrophic out-of-pocket costs for TB care, and integration of health systems for patient-centered care. Each of these goals or outcomes will need to be contextualized to the country and aligned with national strategies and policies. The fostering of a supportive environment, including quality data collection and use, will enable appropriate evaluation of processes and outcomes to determine progress towards sustainable health outcomes.
Acknowledgments
We acknowledge contributions of Elizabeth Eastman and Elyse Callahan for initial background work and review and Sharanya Joshi for review and editing of the final document.
Disclaimer
The authors views expressed in this publication do not necessarily reflect the views of their respective organizations.
References
- Bassili A, Seita A, Baghdadi S, et al. Diagnostic and treatment delay in tuberculosis in 7 countries of the Eastern Mediterranean Region. Infect Dis Clin Pract. 2008; 16(1): 23-35. doi:10.1097/IPC.0b013c31815d8d61
- Heller RF, Gemmell I, Edwards R, et al. Prioritising between direct observation of therapy and case-finding interventions for tuberculosis: Use of population impact measures. BMC Med. 2006; 4: 1-6. doi:10.1186/1741-7015-4-35
- Getnet F, Demissie M, Assefa N, et al. Delay in diagnosis of pulmonary tuberculosis in low-and middle-income settings: Systematic review and meta-analysis. BMC Pulm Med. 2017; 17(1): 1-15. doi:10.1186/s12890-017-0551-y
- Luis SF, Kamp N, Mitchell EMH, et al. Health-seeking norms for tuberculosis symptoms in southern Angola: Implications for behaviour change communications. Int J Tuberc Lung Dis. 2011; 15(7): 943-948. doi:10.5588/ijtld.10.0588
- Bello S, Afolabi RF, Ajayi DT, et al. Empirical evidence of delays in diagnosis and treatment of pulmonary tuberculosis?: systematic review and meta-regression analysis. 2019; 1-11.
- Snyder LB, Hamilton MA, Mitchell EW, et al. A meta-analysis of the effect of mediated health communication campaigns on behavior change in the United States. J Health Commun. 2004; 9: 71-96. doi:10.1080/10810730490271548
- LaCroix JM, Snyder LB, Huedo-Medina TB, et al. Effectiveness of Mass Media Interventions for HIV Prevention, 1986–2013. J Acquir Immune Defic Syndr. 2014; 66: 329-340. doi:10.1097/QAI.0000000000000230
- Collaborative THCC. Malaria Social and Behavior Change Communication Evidence Literature Review. Baltimore MD 2017.
- Vermund SH, Mallalieu EC, Van Lith LM, et al. Health communication and the HIV continuum of care. J Acquir Immune Defic Syndr. 2017; 74: S1-S4. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L613913713.
- Babalola S, Van Lith LM, Mallalieu EC, et al. A framework for health communication across the HIV treatment continuum. J Acquir Immune Defic Syndr. 2017; 74(Supplement 1): S5-S14. http://journals.lww.com/jaids/pages/default.aspx%0Ahttp://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexa&NEWS=N&AN=613913731.
- Roll Back Malaria Partnership to End Malaria. The Strategic Framework for Malaria Social and Behaviour Change Communication 2018-2030. US Pres Malar Initiat. 2018. https://www.pmi.gov/docs/default-source/default-document-library/tools-curricula/framework-for-malaria-social-and-behavior-change-communication-2018-2030-english.pdf].
- Lamstein S, Koniz-Booher P, Beall K, et al. SPRING - Working Paper: SBCC Pathways for Improved Maternal, Infant, and Young Child Nutrition Practices. 2014 September. www.spring-nutrition.org.
- Leslie L, Whang C, Arnold R. A selective literature review on SBCC best practices. 2016 April.
- Kuzari D, Biderman A, Cwikel J. Attitudes of women with breast cancer regarding the doctor-patient relationship. Eur J Cancer Care (Engl). 2013; 22(5): 589-596. doi:10.1111/ecc.12063
- Lestari T, Graham S, Van den Boogard C, et al. Bridging the knowledge-practice gap in tuberculosis contact management in a high-burden setting: a mixed-methods protocol for a multicenter health system strengthening study. Implement Sci. 2019; 14(1): 1-15. doi:10.1186/s13012-019-0870-x
- Warsi S, Elsey H, Boeckmann M, et al. Using behaviour change theory to train health workers on tobacco cessation support for tuberculosis patients: A mixed-methods study in Bangladesh, Nepal and Pakistan. BMC Health Serv Res. 2019; 19(1): 1-14. doi:10.1186/s12913-019-3909-4
- Becker MH. The health belief model and personal health behavior. Health Educ Monogr. 1974; 2(4): 324-473.
- Glanz K, Rimer BK, Viswanath K. Health and Health. 2008. doi:http://hdl.handle.net/2027/spo.10381607.0007.102
- Taylor D, Bury M, Campling N, et al. Nice-Doh Draft Review of Health Behaviour Theories. 2007.
- Reducing Delays in TB Diagnosis: Methods to Evaluate the Frequency and Causes of Delays. TB Care II - Comparative Analysis of Delays in Bangladesh and Swaziland. Uniersity Research Co., LLC. 2012.
- World Health Organization (WHO). A patient-centred approach to TB care. Geneva World Heal Organ. 2018. http://www.who.int/iris/handle/10665/272467.
- Wandwalo ER, Mørkve O. Delay in tuberculosis case-finding and treatment in Mwanza, Tanzania. Int J Tuberc Lung Dis. 2000; 4(2): 133-138.
- Meintjes G, Schoeman H, Morroni C, et al. Patient and provider delay in tuberculosis suspects from communities with a high HIV prevalence in South Africa: A cross-sectional study. BMC Infect Dis. 2008; 8: 1-8. doi:10.1186/1471-2334-8-72
- Kuznetsov VN, Grjibovski AM, Mariandyshev AO, et al. Hopelessness as a basis for tuberculosis diagnostic delay in the Arkhangelsk region: A grounded theory study. BMC Public Health. 2013; 13(1): 1. doi:10.1186/1471-2458-13-712
- White RG, Charalambous S, Cardenas V, et al. Evidence-informed policy making at country level: lessons learned from the South African Tuberculosis Think Tank. Int J Tuberc Lung Dis. 2018 Jun 1; 22(6): 606-613. doi: 10.5588/ijtld.17.0485.
- Public–private mix for TB prevention and care: a roadmap. Geneva: World Health Organization; 2018. License: CC BY-NC-SA 3.0 IGO.
- Uplekar M, Weil D, Lonnroth K, et al. WHO’s new End TB Strategy. Lancet. 2015; 385(9979): 1799-1801. doi:10.1016/S0140-6736(15)60570-0
